Tirohanga Whānui | Overview
The New Zealand Council of Christian Social Services (NZCCSS) welcomes the opportunity to provide feedback on this stage of the Inquiry into Aged Care. We support the kaupapa to address the critical needs in this sector, specifically regarding the supports for those with neurological cognitive disorders.
Many of our members are providers in the aged care sector and have strong concern with the long-term sustainability of support for our most vulnerable older people.
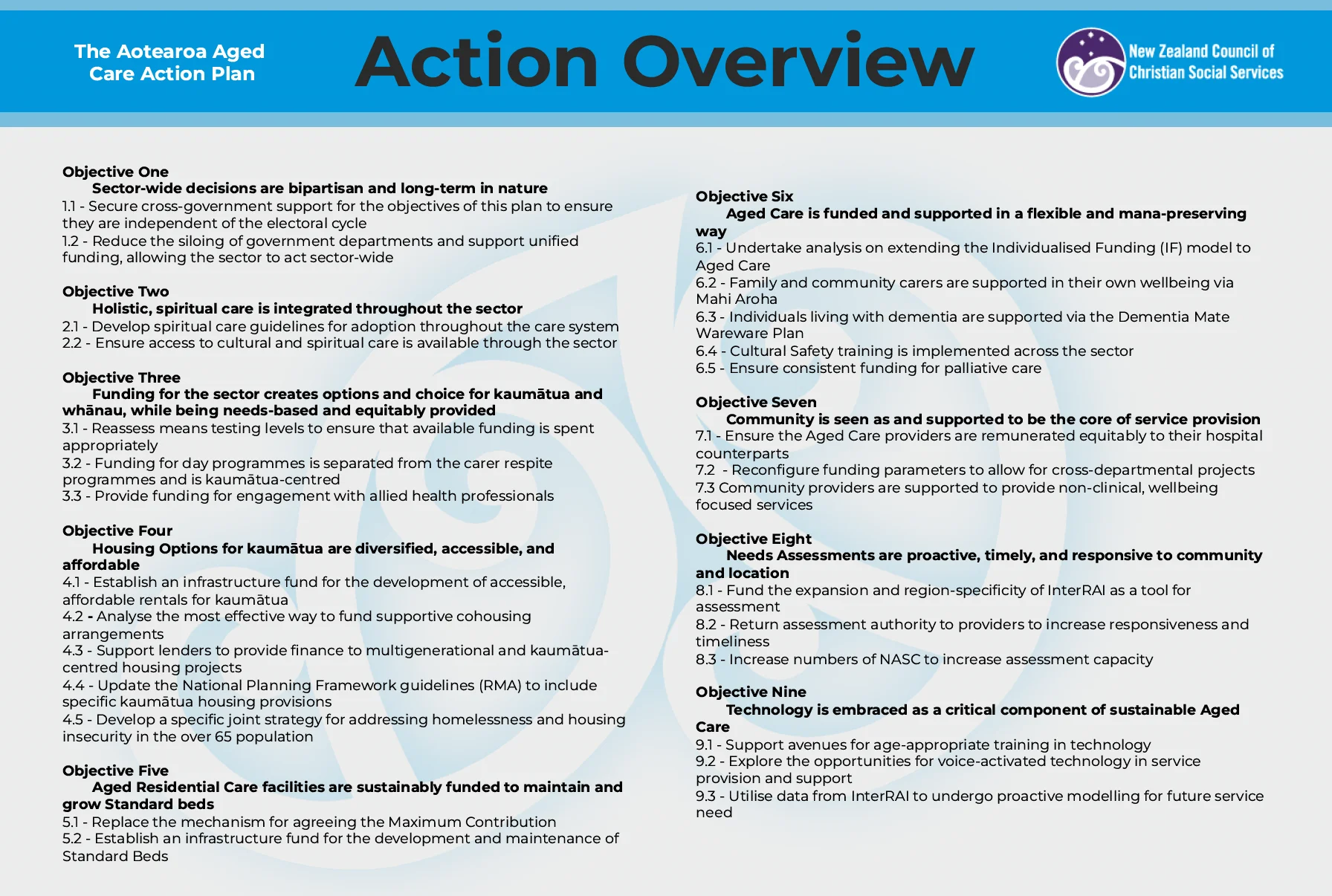
In addition to the points, we have outlined below, we would like to bring our recent work ‘The Aotearoa Aged Care Action Plan’ (AACAP) to the attention of the committee. Where relevant, we have signposted specific actions and objectives of the plan below. We hope that it will assist thinking in this area.
Kaupapa | Purpose
We strongly recommend that the scope of this Inquiry consider the following areas:
- How can we support vulnerable adults to live safely in complex situations?
- How do different parts of Government overlap and interact to ensure the sustainability of this
sector? - How can we ensure that design of the system meets the needs of this cohort?
- How will the increase both in number and complexity of older people be addressed in the
supports? - How will funding be updated to provide meaningful supports for older people and their whānau?
- How will the nuance of age and disability, and the impact of early-onset diagnosis be managed?
- How can we ensure housing is accessible, responsive, available and suitable?
- How will a cultural lens be applied to provide the best support and care for individuals and their
families? - What part does the community have to play? How will this be supported?
- How do cultural implications, including social stigma, impact diagnosis rates and supports?
- How will carers be supported?
Horopaki | Context
1. How can we support vulnerable adults to live safely in complex situations?
Our most vulnerable older adults are often also those who live with the least resources and the least support. In many cases, they are also the ones who live with the most complexity.
While many of these complex individuals are being cared for in aged care homes, many also remain living in the community and some of these individuals will be living alone. Community programmes are the critical lifeline between these individuals and their services, including home help and GPs, but how do we ensure that these services even know that these individuals are there? How do we ensure that the system doesn’t lose those who are the most at risk of falling through its gaps? How do we create a system which supports people who have other intersecting needs? Those who live with additional diagnoses, such as the increasing number of individuals living with Foetal Alcohol Syndrome, and the increasing number of individuals who are ageing with cognitive and learning disabilities, present addition complexities for care. Individuals with a history of drug and alcohol abuse that results in brain damage present significant challenges for caregivers and support programmes, due to being so much younger and more physically able than the other members of the group.
Objective Seven of the AACAP outlines the ways in which community can assist with critical service provision.
2. How do different parts of Government overlap and interact to ensure the sustainability of this
sector?
Government departments are siloed so significantly it hampers innovation and progress. Community organisations that straddle the line between health and social services are constantly pressed between multiple ministries as they battle for support. To create real, transformative change, the way in which Government engages with funding and decision making must be overhauled.
We suggest this begin with an assessment of the Public Sector Finance Act, which enshrines this clear demarcation between sectors in legislation.
Objective One of the AACAP presents actions for ensuring a whole of government approach to
resolving the aged care crisis.
3. How can we ensure that design of the system meets the needs of this cohort?
The system must function in a way that those who need to use it can understand. When we are
considering a system that is being designed to meet the needs of vulnerable older adults who have neurological cognitive disorders, this must be taken into account. The system must be designed and communicated in a way that means those who are being served by it have the best chances of understanding it.
We know how complex the aged care sector is, as we outline in our ‘Aged Care Continuum’:
4. How will the increases both in number and complexity of older people addressed in the supports?
The challenge for aged care is not only our rapidly increasing number of older people, but the dramatic increase in acuity and complexity that individuals are presenting with. The historical balance in service provision between community care, residential rest homes, dementia and hospital levels are in flux. More people, both in volume and in proportion, are requiring the highest levels of care. This must be accounted for at all levels of the service, beginning with needs assessment availability to attempt to catch individuals at lower intervention levels.
Workforce is critical to this, most notably the availability of and workload of Needs Assessment Service Coordinators (NASC). These key individuals are currently acting as a bottleneck for service access, and this issue must be addressed quickly.
Objective Eight of the AACAP gives suggestions on how to ensure that assessments are proactive, timely, and responsive, helping to engage people at lower acuity levels, namely the return of assessment authority to providers to allow NASC to get on with the job of coordinating services.
5. How will funding be updated to provide meaningful supports to older people and their whānau?
Funding for support is complex, difficult to understand, and confusing for many people who do not have someone who can explain the system to them. This can result in people missing out on support they might be entitled to due to misunderstanding or being unable to access the supports that would truly help them due to the heavy restrictions under the current models. Funding must respect the unique nature of each individual and allow them to access services that meet their needs.
Objective Three of the AACAP presents options for how funding can be more flexible, and needs focused for our older people.
6. How will the nuance of age and disability, and the impact of early-onset diagnosis, be managed?
As mentioned above, complexity in aged care is increasing. In many instances, this is as a result of the increasing intersection of age and disability. As a result of medicine and social supports increasing the lifespans of our tāngata wahikaha community, there is now a more significant overlap between disability support and aged care than ever before. This concern overlaps with the increase in early onset diagnosis, and the additional cohort of individuals with brain damage who are more susceptible to cognitive disorders. These groups cannot always be safely cared for in the same setting. The aggression that often accompanies these conditions is more manageable in the aged and frail, but less so in younger and more able-bodied individuals if in the same setting as these older individuals.
These difficulties in management will be critical elements of any system moving forwards, and providers with experience in supporting these cohorts, such as those in our membership, will be critical resources as you navigate this space.
7. How can we ensure housing is accessible, responsive, available and suitable?
Aged residential care is not just a clinical facility, it is a home. It is part of the continuum of housing that we rely on and is only one of the options that must be available.
Housing options must be accessible. Accessibility might be related to how close it is too important elements such as family, healthcare, cultural services. It may also be aspects of the housing itself, such as if it has Universal Design principles that allow individuals with mobility needs to use the house safely. It can also be related to the affordability of the housing. A house with all the perfect accessibility elements that lies outside the affordability of an individual is not accessible at all.
Responsivity is also key. How can individuals move between housing situations as their needs change? This is not only in periods of increasing acuity. Some individuals can regain independence and autonomy when provided with supports, but in many cases the move into an aged care home is a one-way trip. How can we create a system which allows this responsiveness to need?
There are significant differences between regions in terms of population demographics, and older people who live outside major regions are underserved even in areas where they make up a larger section of the population. Understanding where older people live will help in sustainable decision making for this cohort.
Objective Four of the AACAP has some suggestions for supporting housing needs in older people.
8. How will a cultural lens be applied to provide the best support and care for individuals and their families?
Individual needs are intrinsic to the success of their care plan and prognosis, and the cultural and
spiritual needs of a person are core among these needs. Ensuring that there is access to the specific supports a person needs in order to achieve wellness is critical. This wellness can be achieved through engagement with specialised practitioners, such as allied health professionals, and through the supports built into holistic spiritual care.
Objective Two of the AACAP discusses priorities for ensuring spiritual care throughout our aged care sector. Objective Three of the AACAP, specifically Action 3.3, outlines the importance of allied health professionals and funding availability for them.
9. What part does the community have to play? How will this be supported?
Community organisations are the bedrock of support that people rely upon throughout their lives. Never is this truer than where they are providing support to individuals and whanau as they age, with or without neurological conditions. Community groups tether together different programmes, professionals, and supports to ensure people access what they need. In order to do this, community groups must be supported themselves.
Objective Seven of the AACAP outlines how community can be seen and supported to be the core of service provision.
10. How do cultural implications, including social stigma, impact diagnosis rates and supports?
There is a heavy social stigma around many diagnoses, but specifically around neurological and
cognitive diseases. The severity of this stigma varies from culture to culture. In some cases, it is a stigma that affects the individual themselves, and in others it extends to their carer, their family and their wider community. These stigmas make it hard for people to reach out and ask for help in all aspects of the aged care sector, but especially around cognitive conditions.
Overcoming the stigma around help and care in the aged care sector and with cognitive conditions is critical for ensuring that support can get to the people who need it most. Funding for integrated public health campaigns to target this stigma is critical. Investment in this area has strong potential to produce service savings down the continuum as a result of reduced acuity from earlier intervention. This social investment model approach will ensure better distribution of resources and positively impact individuals, their whānau, and the organisations that support them.
11. How will carers be supported?
Mahi Aroha, the Carers Plan, expired at the end of 2023. The previous government did not commit to a renewal, and this government has not yet done so. Carers are critical in the support of all older people, especially those who can remain in their homes and communities. It is estimated that the annual economic contribution of caring, that is the value of care provided free of charge by family members to those who need it, is approximately $17 billion a year in Aotearoa New Zealand, while carers themselves face enormous barriers to access support and income themselves. Committing to renewing and updating Mahi Aroha will enable better support and care for all those who need it, including our older people.
Objective Six of the AACAP, specifically Action 6.2, specifically calls for the renewal of Mahi Aroha to provide this support to carers.
Rauemi | Resources
NZCCSS (2023) Tale of Two Whānau: personalising the effects of the Aged Care Crisis
Ingoa whakapā | Contact Name
Nikki Hurst
Rachel Mackay